What if we could reduce premature deaths by half?
An extraordinary opportunity has emerged in global health. A combination of scientific advancement, healthcare technology and collaborative action has illuminated a future where the possibility of dying before age 70 is half what it was in 2019.
That’s the goal articulated by the Lancet Commission on Investing in Health in its report Global health 2050: the path to halving premature death by mid-century. Halving premature mortality from a baseline set before the pandemic may seem like a lofty ambition, but the Commission lays out a path to achieve it — one where government policy, the work of the research community, and resilient healthcare systems combine so we can move together towards a better future.
“Halving premature death is potentially an incredible achievement — and it’s realistic,” said Sean Cleghorn, Executive Editor at Elsevier journal The Lancet. “The beauty of the report is that it has such an aspirational goal, but it tells you how to get there in a focused, specific manner.”
By identifying and prioritizing 15 critical health conditions, the initiative aims to direct resources and interventions where they are needed most. It not only addresses infectious diseases and maternal health, which are paramount in high-risk countries, but also encompasses a range of non-communicable diseases and injuries that affect people across the globe. It highlights areas for intervention, such as childhood immunization and addressing the spread of infectious diseases, as well as showing how countries can strengthen their health systems and draw on technology to enhance their capacity to deliver essential services.
Mission critical insights for global action
Already, governments around the world are putting the recommendations of the report into action. Dr Gavin Yamey, Professor of the Practice of Global Health at Duke University and one of the collaborators on the Commission, highlighted some examples.
“It’s been very gratifying to see a number of countries explore how the approaches can be applied in their national contexts
"One of the Commissioners, Simiao Chen, is working with planners in Xishui County, China, to use Global Health 2050’s modular health systems strengthening approach to identify key health interventions for scale-up.”
In Denmark, the Danish Alliance for Global Health embraced several of the recommendations in its recent report on the future of Danish global health assistance. Similarly, Norway’s highly influential expert committee on global health has adopted the recommendations in its report Norway can, Norway should: Take the lead in halving premature death by 2050.

Helping impact makers succeed on the frontlines of research
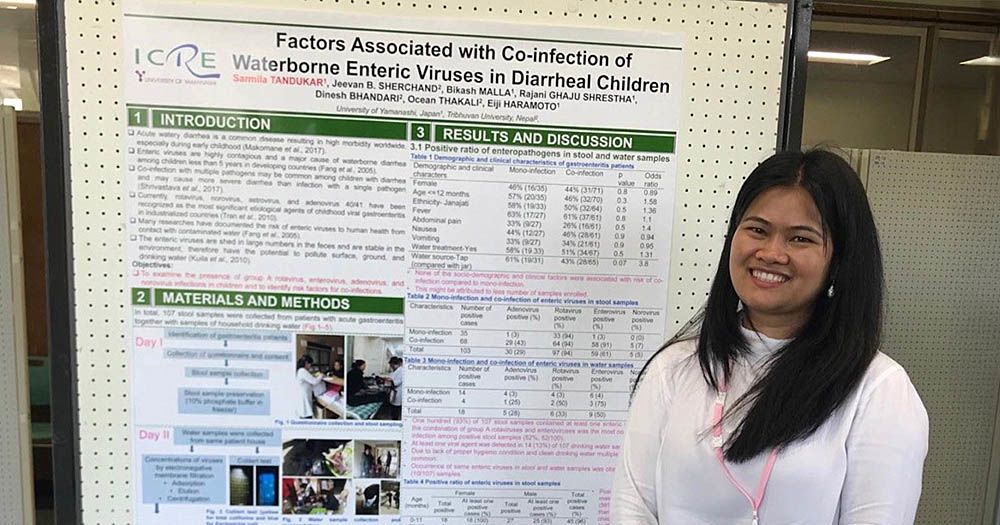
Nepal has launched a national Commission to examine how the report can help guide its national health planning. That’s where Dr Sarmila Tandukar, who won the 2025 OWSD Elsevier Foundation award for inclusive health, does her environmental health research, and she’s been making significant strides in public health in areas identified by the Commission.
Focusing on disease prevention, Sarmila tracks microorganisms and antimicrobial resistance genes (ARGs) to identify emerging health threats in wastewater, sewage, river water and drinking water sources. Her research addresses the spread of diseases including diarrhoea, one of eight infections identified by the report as contributing substantially to the life expectancy gap.
“It’s among the top 10 causes of death in Nepal, particularly affecting children under 5, so tackling diarrhoea gives so many more people a chance at a full life,” Sarmila explained.
Recognizing the need for intervention, Sarmila and her research team focused on understanding the role of waterborne pathogens in disease transmission, and providing critical insights into the environmental factors contributing to high mortality rates. “We wanted to know whether these viruses are present in our water sources,” she said. “And now I’m generating baseline data that is crucial for health policy researchers.”
The Nepalese government has started revising healthcare guidelines based on the findings from researchers like her, and the Lancet Commission recommendations. Her work has been published in multiple Elsevier journals, including Environmental Health and The Lancet Infectious Diseases, bringing it to a global audience of more than 14 million researchers via ScienceDirect. Now, Sarmila is part of a project bringing together researchers from Nepal, Japan, the Philippines and Vietnam to use these tools as an early warning system for infectious diseases and antimicrobial resistance in developing countries.
As Sean noted, it’s a good example of how researchers turn mission critical insights from the report into action at a country level.
“The big-picture elements always need to be tailored for those individual countries, where they have particularly pressing needs. That’s the role researchers play — taking the findings and looking at how they apply to your own national health system and helping guide your government in how it can work in your country.”
Samila Tandukar, PhD, presents her research in Nepal.
Samila Tandukar, PhD, presents her research in Nepal.
Samila Tandukar, PhD
Samila Tandukar, PhD
Enhancing healthcare resilience with technology and innovation
“It’s the combination of cutting-edge tools, comprehensive training and collaborative efforts between public and private sectors that will drive meaningful change.”
Among its recommendations, the Commission highlights the importance of investing in healthcare technology to build the resilience of health systems and drive innovation in medicines, vaccines and diagnostics. One study cited by the report estimates that AI could reduce healthcare costs by 5% to 10%.
Dr Jan Herzhoff, President of Elsevier Health, explained how these tools can contribute to that goal of halving premature mortality:
“Healthcare professionals continue to face growing pressure, working in time-sensitive environments with increasing workloads. They need quick access to trusted, evidence-based information at the point of care. Here, AI can be a true game-changer. Solutions like ClinicalKey AI can dramatically accelerate how physicians find the critical information they need, allowing them to focus more on patient care.”
These tools can also contribute to reducing global health inequality by bringing up-to-date, reliable healthcare information to remote settings:
“Technology can help upskill workers in remote or rural areas. We’re delighted to be working on a significant national pilot in India: the Digital Innovations & Interventions for Sustainable HealthTech Action (DIISHA). This strategic public-private partnership aims to empower and digitally upskill frontline healthcare workers in India, supporting the government’s efforts in building a sustainable rural health system in the country.”
Capacity and training of healthcare professionals is another critical factor in building healthcare resilience. Paul Crockett, Senior VP, in Elsevier’s Nursing and Healthcare Education department, explained some of the challenges.
“Ensuring health systems are appropriately staffed is central to this, and with the World Health Organization estimating a global shortfall of 4.5 million nurses by 2030, recruiting and training more nurses is a critical priority. Capacity in nursing education is a key barrier to recruiting more nurses. Using AI technology to expand personalized learning can play a valuable role in meeting this challenge head on.”
In 2024, Elsevier launched Sherpath AI, the first and most advanced generative AI chat designed for nursing students and faculty. A groundbreaking conversational tool, Sherpath AI gives nursing students access to relevant, personalized content while giving nurse educators tools to help with course preparation and teaching strategies.
Looking to the past for
hope for the future

The possibilities unlocked by technology don’t end there. As Duke University’s Dr Yamey noted, healthcare technology has already led to a massive decline in premature deaths, and there is much more to be gained.
“If you’re looking for reasons to be optimistic about this goal, previous progress from technology is one of them,” he said, pointing to research showing that 80% of the decline in child mortality from 1970 to 2000 in low-and-middle income countries could be attributed to new health technologies.
“Based on what is in the product development pipeline today, the research in the Commission suggests we’ll have around 450 new medicines, vaccines and diagnostics for infectious diseases and maternal health conditions before 2050,” he said.
Technology is accelerating that process. Researchers can search drug approval documents and extracted data with tools like PharmaPendium, visualize biological pathways with EmBiology or go deeper into the bioactivity or molecular level via Reaxys.
For example, chemical and biomolecular engineer Dr Xue Sherry Gao and a team of researchers at Rice University found they could repurpose gene editing technology, called multiplex base-editing, to coax fungi to reveal a larger number of natural compounds — and in a much faster timeframe than previously possible. “These compounds could be useful antibiotics or anticancer drugs,” she explained. “We are in the process of figuring out what the biological functions of these compounds are, and we are collaborating with groups in the Baylor College of Medicine on pharmacological small-molecule drug discovery.
Helping impact-makers succeed worldwide

Those involved in the Lancet Commission’s report continue to present their findings to policymakers at the highest levels.
- Dr Marco Schäferhoff presented the report at a recent dialogue on health investment hosted by Germany’s Federal Ministry for Economic Cooperation and Development (BMZ).
- Commissioner Agnes Soucat spearheaded the launch of a French version of the report at the Nutrition for Growth Summit in Paris.
- A Spanish version is on the way and a launch is planned in Mexico. Gavin and the team continue to work with governments worldwide, along with bilateral and multilateral health and development agencies, to further guide investment in health.
Through this work — put into action by researchers, clinicians and nurses — millions of lives that might otherwise be cut short will have a chance to flourish.
15 priority conditions that cause most premature deaths
The Lancet Commission on Investing in Health proposes that all countries focus on reducing mortality and morbidity from 15 priority conditions, defined using WHO Global Health Estimates. Source: Global health 2050: the path to halving premature death by mid-century, The Lancet (October 2024)
8 infectious and maternal health conditions
- Neonatal conditions: preterm birth complications, birth asphyxia and birth trauma, neonatal sepsis and infections, and other neonatal conditions (e.g., haemorrhagic and haematological disorders, transitory endocrine and metabolic disorders, and digestive disorders)
- Lower respiratory tract infections
- Diarrhoeal diseases
- HIV/AIDS
- Tuberculosis
- Malaria
- Childhood cluster diseases (all vaccine-preventable): Whooping cough, diphtheria, measles, tetanus
- Maternal conditions
7 NCD and injury-related conditions
- Atherosclerotic cardiovascular diseases: Ischaemic heart disease and ischaemic stroke
- Haemorrhagic stroke
- NCDs strongly linked to infections: Stomach cancer, liver cancer secondary to infection with hepatitis B virus or hepatitis C virus, cervical cancer, rheumatic heart disease, and cirrhosis due to infection with hepatitis B virus or hepatitis C virus.
- NCDs strongly linked to tobacco use: Chronic obstructive pulmonary disease (COPD) and cancers of the mouth, oropharynx (lip and oral cavity, nasopharynx, and other pharynx), trachea, bronchus, lung and larynx (Tobacco-related deaths from atherosclerotic cardiovascular diseases and haemorrhagic stroke are included in those categories.
- Diabetes: Including chronic kidney disease due to diabetes
- Road injury
- Suicide